FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are specific types of carbohydrates that are difficult for the body to digest and can cause discomfort for people with irritable bowel syndrome (IBS) who may be sensitive to one or more of them. FODMAPs are found in fruits, vegetables, grains, legumes, and dairy products. Since we know that vegetables, fruits, legumes, and whole grains are good sources of fiber, it may be difficult to determine what foods to eat to help meet daily fiber needs when beginning or maintaining a low FODMAP diet. However, it is imperative not to compromise on your fiber consumption, because it plays an important role in maintaining gut health and overall health. The good news is, there are many low FODMAP foods that contain a significant amount of fiber that can help you meet your daily goal. Let’s dive into some strategies for incorporating more fiber into your low FODMAP diet.
The first strategy is to choose low-FODMAP fiber sources. Some low-FODMAP vegetables include carrots, zucchini, green beans, and potatoes, while some low-FODMAP fruits include strawberries, blueberries, kiwis, and oranges. Grains such as oats, quinoa, and brown rice are low-FODMAP options that contain significant amounts of fiber. Some additional high-fiber, low-FODMAP foods include chia seeds, flax seeds, and nuts such as almonds, peanuts, or pecans.
The next strategy is to manage portion sizes. When starting to add more fiber into the diet while experiencing sensitivity to FODMAPs, it is important to make sure that the fiber foods you are consuming are eaten in portion sizes that fall within the green level of FODMAP content. To increase the amount of fiber foods that you are able to tolerate in one sitting, try to eat small servings of several different fiber foods rather than relying on a large serving of a single food to provide the fiber for your meal. When we do this, we are helping to avoid FODMAP stacking, which can cause GI upset. Additionally, it can be helpful to spread out fiber intake evenly throughout the day instead of focusing on high-fiber foods during only one meal or snack. Your digestive system will be much happier if it is not receiving all of your daily fiber needs at once.
The last strategy is to be mindful of ways to reduce FODMAP content when cooking or preparing foods. Pickling certain higher FODMAP foods such as onions, garlic, and beets has been shown to reduce their FODMAP content by up to 80%1 making them suitable for a low FODMAP diet. Beets are high in fiber, so this is a great option that may work for you if you can tolerate beets. Certain cooking methods such as boiling can also help to reduce FODMAP content in certain foods. For example, boiling legumes such as lentils, or beans can reduce their FODMAP content and may make them more tolerable, especially if they are pre-soaked. Alternatively, if you are in a crunch for time and soaking and boiling legumes isn’t an option, canned legumes such as beans and chickpeas have been shown to contain lower levels of FODMAPs compared to their dried counterparts.
Whether you have been diagnosed with IBS or just have come to notice an intolerance to a certain group of FODMAP, it is important to make sure your fiber intake is adequate in order to help keep your bowel movements regular, support healthy cholesterol levels, increase satiety, and possibly help with blood sugar regulation.
Here is a list of some common foods along with their fiber content in a low FODMAP portion:2,3
- Chia seeds- 2 Tbsp= 10g fiber
- Mung beans- ¼ cup= 8g fiber
- 2 mandarin oranges- 6g fiber
- Kiwi- 2 medium kiwis= 5g of fiber
- Quinoa- 1 cup cooked= 5g fiber
- Gluten-free seed/grain bread. One brand of gluten-free bread that has a high-fiber option is Schar. Look for the multigrain or grain and seed bread sandwich breads with contain 5g of fiber per 2 slices.
- 2 slices is considered a low FODMAP serving
- Oatmeal- ½ cup oats (measured dry)= 4g fiber
- Potato with skin- 1 medium potato= 4g fiber
- Canned lentils- ¼ cup= 5g fiber
- Brown rice- 1 cup cooked= 3.5g fiber
- Raspberries- ½ cup= 3.5g fiber
- Chickpeas- ¼ cup = 3g fiber
- Flaxseeds / Flaxmeal- 1 Tbsp= 3g fiber
- Eggplant- 1 cup= 2.5g fiber
In conclusion, maintaining a low FODMAP diet while ensuring adequate fiber intake may seem challenging, but it’s absolutely achievable when the right approach is taken. By choosing foods that are low FODMAP, but also good sources of fiber, controlling portion sizes of foods that may cause some discomfort in larger quantities, and preparing foods mindfully, you can reap the benefits of a fiber-rich diet without triggering unpleasant digestive symptoms.
If you’re out of ideas, try one of these low FODMAP, high fiber recipes:
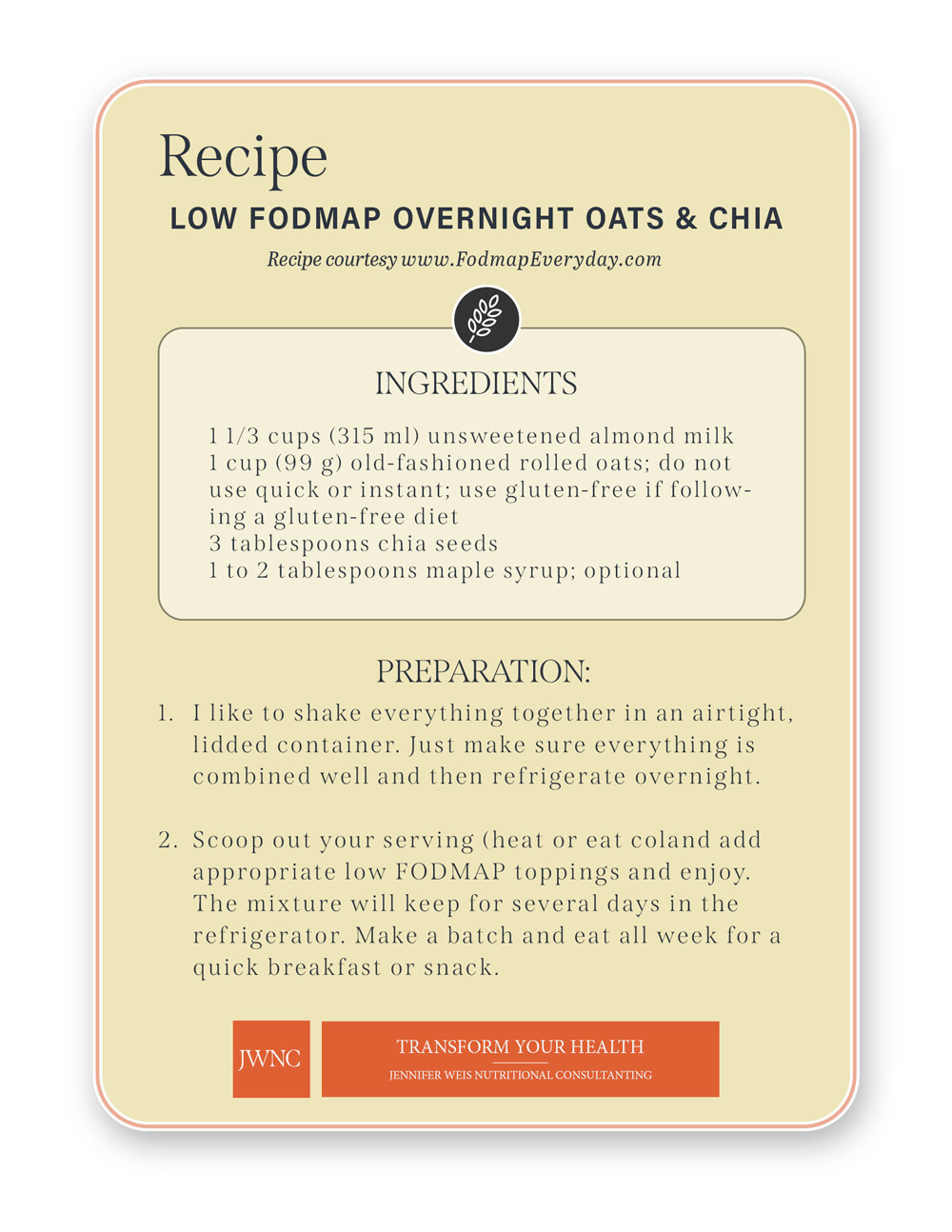
Breakfast: Low FODMAP Overnight Oats– contains 6g fiber per serving
Lunch: Low FODMAP Quinoa Chickpea Bowl– contains 4g fiber per serving
Dinner: Low FODMAP Lentil Dahl– contains 8g fiber per serving
References:
- Dewell A. 5 Ways to Lower the FODMAP Content of Foods: Effect of Food Processing Techniques. Antonella Dewell. Published September 25, 2018. Accessed October 30, 2023.
- Fody Foods. A Guide to High Fiber, Low FODMAP Foods | Fody Food Co. FODY Food Co. – USA. Accessed October 30, 2023.
Monash University. Low FODMAP Diet | IBS Research at Monash University. Monash Fodmap. Monashfodmap.com. Published 2019.